Updated October 12, 2025
Workers’ Comp and Surgery: The Truth About Settlements in California
"Does workers comp pay for surgery?" This question weighs heavily on the minds of injured California workers facing the prospect of expensive medical procedures. Surgery after a workplace injury can cost tens of thousands of dollars—leaving many wondering if they'll be financially responsible for these necessary treatments.
The truth is, workers' compensation in California generally does cover medically necessary surgeries, however, the process is rarely straightforward. From obtaining approval to understanding how surgical procedures affect your settlement value, navigating the workers' compensation system while dealing with a serious injury can feel overwhelming.
In this comprehensive guide, we'll explore exactly what surgical procedures workers' comp covers in California, how these procedures impact your settlement value, and the critical timing considerations that could significantly affect your financial recovery. Whether you're preparing for surgery or have already undergone a procedure, understanding these factors is essential for protecting your rights and securing the compensation you deserve.
How Workers’ Comp Covers Surgery in California
California's workers' compensation system provides a safety net for employees injured on the job. Understanding exactly what surgical procedures are covered and how to get them approved is crucial for injured workers facing potential operations.
What workers' comp typically pays for
In California, workers' compensation insurance covers all reasonable and necessary medical treatments related to workplace injuries, including surgical procedures. This coverage extends to a wide range of operations—from relatively minor procedures like carpal tunnel release to major surgeries such as spinal fusions.
The system aims to provide comprehensive medical care that helps injured workers recover and return to work. This includes not just the surgery itself, but also:
- Pre-surgical consultations and diagnostic tests
- Hospital stays and facility fees
- Anesthesia services
- Post-surgical medications
- Physical therapy and rehabilitation
- Follow-up appointments
- Medical equipment needed during recovery
Additionally, workers' comp covers reasonable travel expenses to and from medical appointments, including surgeries. This ensures that geographic location doesn't become a barrier to receiving necessary care.
When surgery is considered medically necessary
Not every requested surgery receives automatic approval. For a surgical procedure to be covered, it must be deemed "medically necessary" by specific standards. This determination typically requires:
- Documentation showing the injury is work-related
- Evidence that non-surgical treatments have been tried and failed
- Medical records indicating surgery offers a reasonable chance of improving the worker's condition
Medical necessity is established primarily through the treating physician's recommendations. Nevertheless, insurance carriers often scrutinize these recommendations, particularly for expensive procedures like spinal surgeries or joint replacements.
Furthermore, the timing of surgical recommendations matters. California's workers' compensation guidelines generally recommend conservative treatment approaches before considering surgery. This means injured workers may need to try medication, physical therapy, or other non-invasive treatments before surgery is approved.
How approval for surgery works
The surgery approval process in California workers' compensation follows a structured pathway. First, the treating physician—who must be within the employer's Medical Provider Network (MPN) unless properly predesignated—recommends the surgery and submits a request.
This request then undergoes Utilization Review (UR), where medical professionals review the recommendation against evidence-based guidelines. The UR process must be completed within specific timeframes:
- 72 hours for urgent requests
- 5 business days for non-urgent requests
If denied through UR, the injured worker can appeal through Independent Medical Review (IMR). During this process, an independent physician reviews the case and makes a binding determination about medical necessity.
Throughout this approval journey, clear communication between the injured worker, treating physician, and claims administrator is vital. Delays often occur when documentation is incomplete or when there are questions about the connection between the workplace injury and the need for surgery.
Securing surgical approval requires patience and persistence, but understanding these steps helps injured workers navigate the system more effectively.
How Surgery Affects Your Settlement Value
Undergoing surgery for a work-related injury dramatically changes the landscape of your workers' compensation claim. When surgical intervention becomes necessary, several factors come into play that can substantially increase your potential settlement value.
Surgery increases medical costs
Surgical procedures represent some of the most significant expenses in workers' compensation claims. The cost of a single surgery can range from a few thousand dollars to well over $100,000 depending on the type, location, and severity of the injury [1]. For instance, herniated disk surgery—a common procedure for workplace back injuries—can cost upwards of $35,000 [1].
These substantial medical expenses factor directly into your settlement calculations. Your settlement must account for all reasonable and necessary medical treatments related to your workplace injury [2]. Essentially, higher medical bills translate to higher settlement offers, as insurance companies must consider these actual expenses when determining compensation.
Higher impairment ratings after surgery
One of the most significant ways surgery affects your settlement is through impairment ratings—the medical assessment of your permanent limitations. Data shows a clear correlation between surgeries and higher impairment ratings:
- Workers with no surgeries receive an average impairment rating of 5% [3]
- Those with one surgery average 6.6% impairment (1.6 points higher) [3]
- Workers with two surgeries average 8.2% impairment (3.2 points higher) [3]
- Those with three or more surgeries average 11.3% impairment (6.3 points higher) [3]
These higher ratings directly impact permanent disability benefits, which compensate you for lasting limitations that affect your ability to work. Consequently, more extensive surgical intervention often leads to more substantial settlements.
Longer recovery means more lost wages
Surgical recovery typically requires extended time away from work, increasing your eligibility for temporary disability benefits. In California, temporary disability payments generally provide two-thirds of your pre-injury wages while you're unable to work [2].
Recovery timelines significantly impact settlement values. Claims reaching maximum medical improvement (MMI) in less than six months result in average impairment ratings of approximately 5%, whereas claims taking more than two years—often involving surgeries—result in average impairment ratings around 11% [3].
Moreover, California law allows temporary disability benefits for up to 104 weeks within a five-year period from your injury date [2]. Surgical intervention frequently extends this disability period, maximizing the wage replacement portion of your settlement.
Future care and follow-up treatments
Perhaps most importantly, surgery often necessitates ongoing medical care. Your settlement must account for these future medical needs, including:
- Post-surgical rehabilitation and physical therapy
- Follow-up surgical procedures for complications
- Prescription medications for pain management
- Medical devices or equipment needed long-term
- Future doctor visits and monitoring
Insurance companies carefully assess your medical records and consult with doctors to estimate these future care costs [4]. Conditions expected to worsen over time could further increase your settlement value [4].
In practical terms, this means the initial settlement offer without surgery might be around $50,000, yet with surgery and its associated costs, future medical needs, and potential earnings impact, that same claim could result in a settlement of $150,000 [5].
Indeed, insurance companies recognize that surgery typically indicates a more serious injury with longer-lasting consequences. Though no settlement calculation follows a simple formula, the presence of surgery in your claim fundamentally alters its value by increasing all major compensation factors: medical expenses, disability ratings, lost wage periods, and future care requirements.
Timing Matters: Before or After Settlement
The timing of your surgery in relation to your workers' compensation settlement represents a critical decision that significantly impacts your financial and medical future. Understanding who pays for what—and when—can make the difference between adequate coverage and potentially devastating out-of-pocket expenses.
Surgery before settlement: what's covered
When surgery occurs prior to settlement, workers' compensation typically covers all reasonable and necessary medical costs related to your workplace injury. Workers have the right to medical care for job-related injuries until they reach maximum medical improvement. This includes surgical procedures recommended by authorized physicians within the employer's provider network.
Initially, your employer's insurance carrier must authorize the surgery following a utilization review process. Once approved, they cover the surgical costs, hospital stays, medications, and rehabilitation services. This approach ensures you receive needed medical care without upfront expenses, although you may have less control over provider selection.
Surgery after settlement: who pays?
The answer to this crucial question depends entirely on what type of settlement you accept. California offers two primary settlement options with dramatically different implications for post-settlement surgery:
Stipulation with Request for Award (Stips): With this settlement type, you retain the right to lifetime medical care for your injury. The insurance company remains responsible for covering future surgeries and treatments, provided they relate to your documented workplace injury. You can even reopen your claim within five years of the injury date if your condition worsens.
Compromise and Release (C&R): Under this lump-sum settlement, you receive all compensation at once—including an estimate for future medical expenses. Subsequently, you become responsible for paying all future medical costs, including surgeries. The insurance company has no further obligation once you sign this agreement.
Risks of settling before surgery
Accepting a settlement—especially a Compromise and Release—prior to having recommended surgery carries substantial risks:
Unpredictable complications: If surgical complications arise after settlement, you'll bear those additional costs without further compensation. Even careful estimates can't predict every possible outcome.
Permanent restrictions: Post-surgical work restrictions that emerge after settlement cannot generate additional disability benefits once your case is closed through a C&R.
Inaccurate cost projections: The estimated surgery costs included in your settlement might fall short of actual expenses, particularly as medical costs continue rising.
Limited recourse: After accepting a C&R settlement, you generally cannot reopen your claim—even if your condition deteriorates and requires more extensive treatment than anticipated.
Despite these risks, settling before surgery does offer certain advantages, including freedom to choose your own surgeon and scheduling flexibility. Additionally, if you have access to other health insurance that might cover the procedure, you could potentially benefit financially from including the projected surgical costs in your settlement.
The decision ultimately requires careful consideration of your specific circumstances, medical condition, and financial situation—preferably with guidance from an experienced workers' compensation attorney who can evaluate the long-term implications of your choices.
Types of Workers’ Comp Settlements in California
When confronted with a workplace injury requiring surgery, California workers must understand the two distinct settlement options available to them. Each settlement type carries unique implications for medical coverage, especially regarding surgical procedures.
Compromise and Release explained
A Compromise and Release (C&R) settlement functions as a complete buyout of your workers' compensation claim. Under this arrangement, you receive a one-time lump sum payment that covers:
- All future medical care related to your injury
- Permanent disability benefits
- Any temporary disability payments still owed
Once you accept a C&R, the insurance carrier is released from all future liability. This means you become solely responsible for managing your medical care, including any surgeries. The settlement amount typically includes calculations for anticipated medical expenses based on your condition and treatment history.
A key advantage of C&R settlements is immediate access to a larger sum of money, offering financial flexibility. Yet this comes with the significant trade-off of assuming all risk for future medical complications.
Stipulation and Award explained
Alternatively, a Stipulation and Award (Stips) keeps your medical benefits open for life. This settlement type:
- Provides permanent disability benefits in biweekly payments rather than a lump sum
- Maintains the insurance company's responsibility for all reasonable medical care
- Allows for reopening your case within five years if your condition worsens
With Stips, the insurance carrier continues covering medical treatments, including necessary surgeries, indefinitely—provided they relate to your documented workplace injury. This ongoing coverage offers long-term security, albeit with continued insurance company oversight of your medical decisions.
Which is better if surgery is involved?
For injuries requiring surgery, the question of optimal settlement type hinges on timing and certainty. If you've already completed surgery with successful results and minimal likelihood of complications, a C&R might be advantageous—you'll receive compensation for future care you may not need.
Conversely, if you're facing surgical uncertainty—perhaps requiring multiple procedures or having high risk of complications—a Stipulation and Award provides crucial protection. This becomes particularly important with complex operations like spinal fusions or joint replacements where outcomes remain unpredictable.
Beyond merely, does workers comp pay for surgery, you must consider who controls these decisions. With Stips, the insurance company retains approval authority for surgical procedures, sometimes creating delays or denials. Under a C&R, you gain decision-making freedom but shoulder the financial burden entirely.
How Much Can Surgery Increase a Settlement?
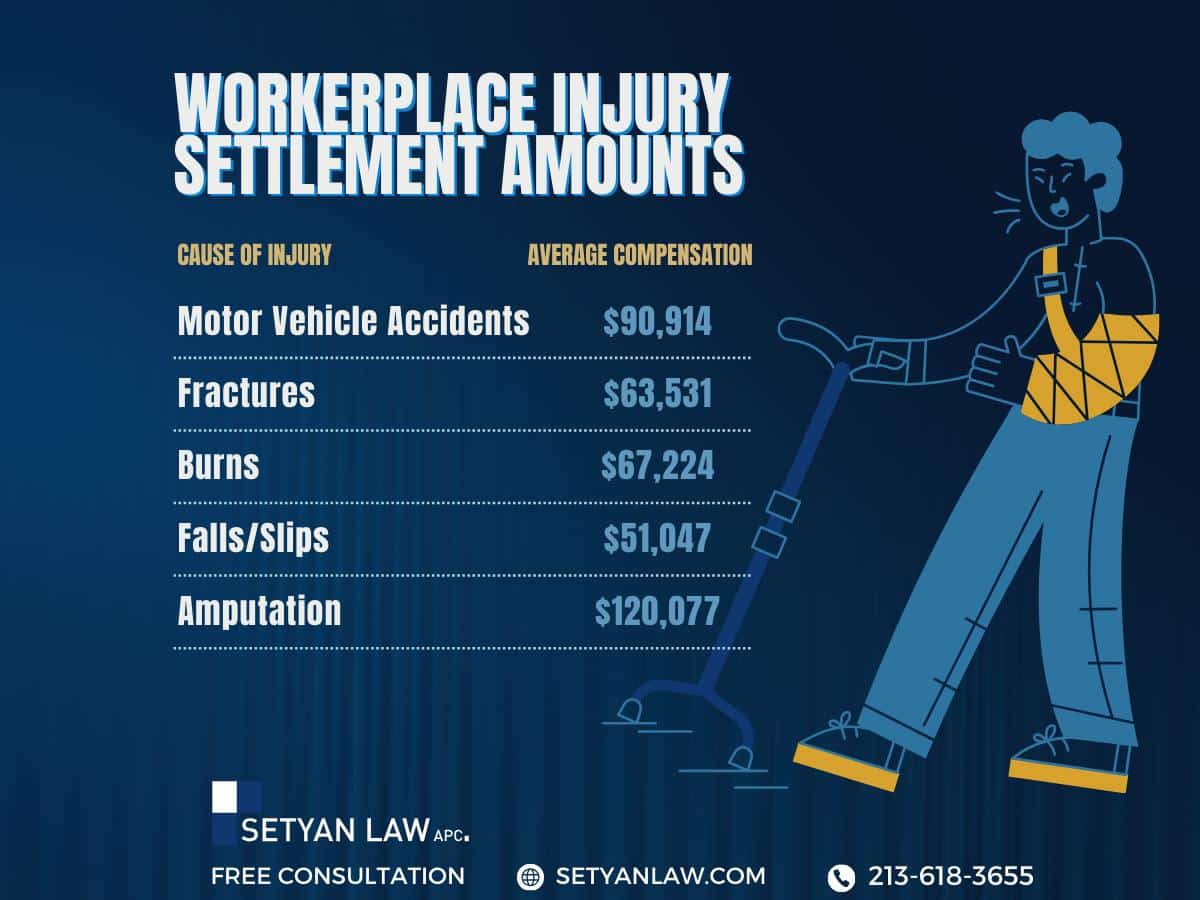
Surgical procedures dramatically influence workers' compensation settlements, often serving as the single most significant factor in determining final payment amounts. Knowing the potential value increase can help injured workers make informed decisions about their claims.
Examples of common surgeries and costs
The financial impact of surgery varies based on procedure complexity. Spinal fusion surgeries for serious back injuries average $110,000 [6], making them among the costliest workplace injury treatments. Joint replacement surgeries typically range from $16,500 to $33,000 [6], while surgeries for broken wrists average around $8,000 [6]. Other common procedures include carpal tunnel surgery, ACL reconstruction, rotator cuff repairs, and neurological surgeries that can exceed $100,000 [7] in complex cases.
Impact of complications or permanent disability
Surgical complications or unsuccessful outcomes substantially increase settlement values. In fact, failed surgeries often necessitate revision procedures, extending recovery time and potentially resulting in permanent disability. A higher impairment rating directly translates to larger settlements [8]. Importantly, a surgery indicating ongoing medical needs—including follow-up visits, additional therapy, or potential revision procedures—becomes a critical factor in negotiations [8]. Age likewise affects settlements, as younger workers with longer disability periods typically receive higher compensation [9].
Geographic cost differences in California
Surprisingly, identical surgical procedures cost significantly different amounts depending on location within California [10]. The average hospital stay in California costs $4,181 per day [6], substantially higher than the national average of $2,883 [6]. These regional cost variations reflect broader economic patterns throughout the state, with treatment in major metropolitan areas typically commanding premium rates. Consequently, settlement amounts often incorporate these geographical considerations when calculating appropriate compensation.
Conclusion
Understanding how workers' compensation covers surgery represents a critical factor for injured California workers. Throughout this article, we've explored the complex relationship between surgical procedures and workers' comp settlements. Workers facing work-related injuries can take comfort knowing their necessary surgeries are typically covered, though approval processes remain rigorous.
Surgery fundamentally transforms the value of a workers' compensation claim. Medical costs, higher impairment ratings, extended recovery periods, and future care needs all contribute to substantially increased settlements. A claim worth $50,000 without surgery might reach $150,000 or more with surgical intervention.
The timing of your surgery relative to settlement carries significant financial implications. Surgery before settlement ensures coverage through the workers' compensation system, whereas post-settlement surgery costs depend entirely on your settlement type. A Compromise and Release leaves you responsible for all future medical expenses, while a Stipulation with Request for Award maintains lifetime coverage for your work injury.
Each settlement option offers distinct advantages based on your specific situation. Injured workers must carefully weigh immediate financial needs against long-term medical considerations, especially when surgery factors into their recovery. Geographic location within California also affects surgery costs and, consequently, settlement values.
Ultimately, surgical procedures represent both a medical necessity and a financial consideration for injured California workers. Armed with this knowledge, you can make more informed decisions about your workers' compensation claim and secure appropriate compensation for your workplace injury. Consultation with an experienced workers' compensation attorney still remains your best strategy when navigating these complex decisions, particularly when surgery becomes part of your recovery journey.
References
[1] – https://www.samndan.com/resources/average-workers-compensation-settlement/
[2] – https://www.dir.ca.gov/dwc/wcfaqiw.html
[3] – https://www.ncci.com/Articles/Documents/Impairment-Ratings-Research_Final.pdf
[4] – https://mehtamcconnell.com/blog/workers-comp-future-medical-buyout-calculator/
[5] – https://www.lawlinq.com/does-surgery-increase-workers-comp-settlement-in-california/
[6] – https://www.shouselaw.com/ca/blog/does-surgery-increase-workers-comp-settlement/
[7] – https://www.fendonlaw.net/blog/does-surgery-increase-workers-comp-settlement/
[8] – https://coronasummitsc.com/does-outpatient-surgery-increase-your-workers-comp-settlement-a-complete-guide/
[9] – https://www.hansfordlawfirm.com/blog/2024/july/does-surgery-increase-your-workers-comp-settlement/
[10] – https://www.wcirb.com/sites/default/files/documents/frictional_cost_report-ar_0.pdf
Call Setyan Law at (213)-618-3655 for a consultation.